Thyroid surgery is performed for a variety of conditions, and there are specific indications for each type of operation. However, like any surgery, thyroid procedures come with certain risks.
The main risks of thyroid surgery involve potential damage to vital structures near the thyroid, particularly:
- Parathyroid glands (which regulate calcium levels in the body)
- Recurrent and external laryngeal nerves (which control the vocal cords)
Thyroid enlargement (goitre)
Goitre simply means an enlargement of the thyroid gland. It is not in itself a diagnosis. Both physiological and pathological conditions may cause a goitre.
Simple goitre
This is a diffuse enlargement of the thyroid and may result from iodine deficiency. Diffuse enlargement of the gland also occurs in Graves disease.
Multinodular goitre
This benign goitre is the commonest thyroid problem. It is caused by episodic periods of thyroid hypo function and subsequent thyroid stimulating hormone hyper secretion which leads to hyperplasia of the gland. This is followed by involution of the gland. Prolonged periods of hyper-plasia and involution are thought to be responsible for the nodular enlargement of the gland found in a multi nodular goitre. A finding of a single nodular enlargement of the thyroid raises the question of malignancy.
Treatment
A partial thyroidectomy may be necessary but only in a patient with one or all of the following signs:
- Pressure symptoms in the neck
- Dysphagia
- Airway compression
- Cosmetic deformity
Graves disease
This is an auto-immune condition where antibodies are produced which mimic the effect of TSH. A hyperthyroid state develops and there is often a smooth goitre. The patient’s eye signs may be most impressive.
Treatment
Hormonal manipulation with carbimazole. Surgery to correct the proptosis may be achieved via a trans-nasal orbital decompression. Here, the medial wall of the bony orbit is removed to allow the orbital contents to herniate into the nasal cavity.
Hashimoto thyroiditis
This is an auto immune condition where there is often hyperthyroidism and many patients develop a goitre. Thyroxine replacements may be necessary. Patients with this condition have an increased risk of developing a thyroid lymphoma.
Thyroid Neoplasia
Thyroid tumours may arise from either the follicular cells or the supporting cells found in the normal gland. They are quite common and each of these tumours has its own particular characteristics. Papillary and follicular adenocarcinomas are frequently referred to as differentiated thyroid tumours.
Follicular cell neoplasms
- Papillary adenocarcinoma
- Follicular adenocarcinoma
- Anaplastic adenocarcinoma
Supporting cell neoplasms
- Medullary carcinoma
Papillary adenocarcinoma
These usually affect adults age 40-50 years. There are usually multiple tumours within the gland. 60% of affected patients have involved neck nodes. If the disease is limited to the gland, 90% of patients will survive 10 years or more. If the disease has spread to involve the neck nodes 60% of patients will survive 10 years or more.
Treatment: Involves a near total thyroidectomy. Plus a neck dissection where there are involved nodes. Post operative radio-iodine may be given to ablate any viable thyroid tissue or tumour left behind after the surgery. After surgery, patients will need life-long thyroid replacement at TSH suppressing doses.
Follicular adenocarcinoma
It usually affects adults age 50-60 years. There is a well defined capsule enclosing the tumour and it spreads via the bloodstream. Up to 30% of patients will have distant metastases at presentation and hence to prognosis is less good than in papillary adenocarcinoma.
Anaplastic thyroid carcinoma
This condition occurs in adults over 70 years of age, and is more common in women. It involves rapid enlargement of the thyroid gland and pain. The patient will have airway, voice or swallowing problems due to direct involvement of the trachea, larynx or oesophagus. The prognosis is very poor. 92% of patients with this condition will die within 1 year, even with treatment.
Medullary carcinoma
This arises from the parafollicular C cells (or calcitonin secreting cells) The patients level of serum calicitonin is raised and their serum calcium level remains normal. Neck metastases are present in up to 30% of patients.
Treatment: Involves a near total thyroidectomy and radiotherapy.
Benign thyroid adenoma
These can be functioning adenomas or non functioning adenomas:
Functioning adenomas
They produce thyroxine and will take up iodine and technetium. They appear bright or ‘hot’ on isotope scanning. Symptoms of thyrotoxicosis may develop. They are rarely malignant. Treatment is usually medical via thyroid suppressing drugs, but may be treated surgically via excision. Radiotherapy and ablation may be required.
Non-functioning adenomas
These adenomas do not take up iodine. They appear ‘cold’ on isotope scanning. 10-20% will be malignant. Treatment will be via a surgical excision.
Treatment of Thyroid conditions
Management of a thyroid lump
Management of a thyroid lump (nodule) depends on whether it’s benign or cancerous, and its size and symptoms. For benign nodules, options include observation, surgery for large or symptomatic nodules, or radiofrequency ablation (RFA). For cancerous nodules, surgery (thyroidectomy) is usually the primary treatment, potentially followed by radioactive iodine treatment.
Hormonal manipulation
Thyroxine: Patients experiencing hypothyroid states and after thyroidectomy may need to take thyroxine for life. Doses of thyroxine sufficient to suppress the TSH production are given in well differentiated thyroid cancers in order to reduce tumour growth since these tumours are also TSH driven.
Carbimazole or propylthirouracil: May be given in hyperthyroidism since these inhibit the formation of T3 and T4.
Radioactive ablation
Most well differentiated thyroid tumours will trap iodine. This ability can be put to therapeutic effect by administering radioactive iodine. The patient is first rendered hypothyroid by thyroidectomy. The tumour cells then become hungry for iodine and as such will avidly take up the radioactive iodine to their own cytotoxic demise! Radio-iodine therapy can also be used to control a persistent hyperthyroid state.
Thyroid surgery
Thyroid surgery is generally safe and well tolerated by patients.
Hemithyroidectomy: This involves the removal of one thyroid lobe. It is indicated in benign thyroid conditions and as an excisional biopsy procedure where malignancy is suspected but not confirmed.
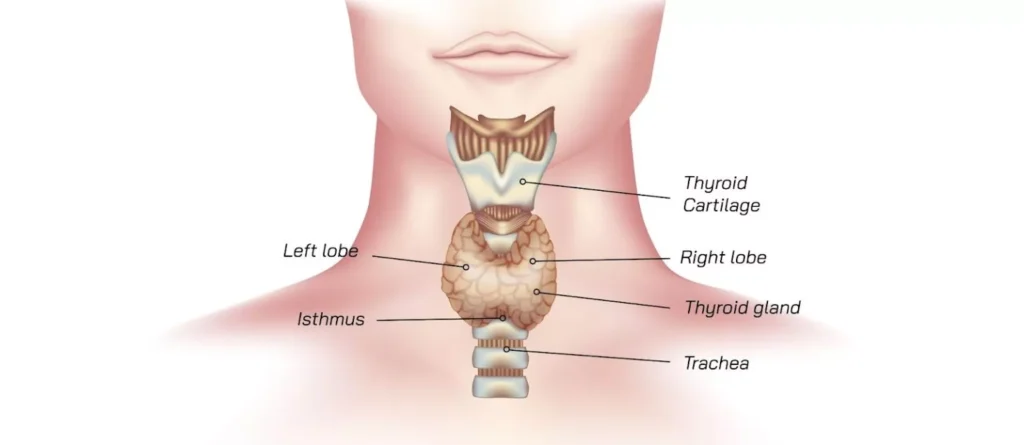
Total thyroidectomy: This is indicated in thyroid malignancy. Because it increases the risks to the recurrent laryngeal nerves and to the parathyroid glands, some surgeons will perform a near total thyroidectomy, leaving a small amount of thyroid tissue behind in the area of the recurrent laryngeal nerve.
Risks of Thyroid surgery
These are some of the most common and important risks of thyroid surgery:
Vocal cord palsy
though stretching of the nerve can cause transient vocal paresis, which improves over few weeks, but sometimes this is due to recurrent laryngeal nerve damage. Patients will present with a weak and breathy voice. All patients should undergo a vocal cord check pre operatively to document cord mobility before the procedure.
Bilateral vocal cord palsy
This will lead to medialisation of the vocal cords resulting in life threatening airway obstruction. Facilities for reintubation and tracheostomy must be readily available.
Haematoma
Haematoma after thyroid surgery is another potentially serious complication. This is because the vascular nature of the thyroid can lead to a rapid accumulation of blood in the neck, resulting in compression of the airway. If a patient’s neck begins to swell rapidly after thyroid surgery, the wound is re-opened, the clot evacuated and the airway restored. Once the airway has been secured, the bleeding point can be found and controlled.
Hypocalcaemia
This should be anticipated whenever a total thyroidectomy has been performed. Calcium levels should be checked and the patient should be observed for the signs of hypocalcaemia such as:
- Tingling in the hands and feet
- Perioral paraesthesia
- Muscle cramps
- Carpopedal spasm muscle spasms affecting the hands and feet
- Chvosteck’s sign facial spasm seen on tapping over the facial nerve in the region of the parotid
- Tetany generalized muscle spasm.
As soon as hypocalcaemia is suspected, oral replacement therapy and at times IV calcium gluconate may be necessary.
Parathyroidectomy
Parathyroidectomy is surgery to remove one or more of the parathyroid glands or a tumor that’s affecting a parathyroid gland.
Parathyroid glands are four tiny structures, each about the size of a grain of rice. They are located behind the thyroid at the bottom of the neck. These glands make parathyroid hormone. That hormone helps keep the right balance of calcium in the bloodstream, as well as in body tissues that need calcium to work correctly. Parathyroid hormone is essential for nerves and muscles to work properly and for bones to be healthy.
Parathyroidectomy often is done to treat overactive parathyroid glands, a condition called hyperparathyroidism. In many cases, only one of the parathyroid glands need to be removed to effectively treat hyperparathyroidism.
Risks of Parathyroidectomy
- Injury to the thyroid gland or the need to remove part of the thyroid gland.
- Hypoparathyroidism (parathyroid glands not producing enough parathyroid hormone). This can lead to low calcium levels that are dangerous to your health.
- Injury to the nerves going to the muscles that move your vocal cords. You may have a hoarse or weaker voice which could be temporary or permanent.
- Difficulty breathing. This is not common and usually goes away several weeks or months after surgery.
Potential problems that could happen after this surgery include:
- Infection
- A collection of blood (hematoma) under the skin of the neck that causes swelling and pressure
- Long-term low calcium levels due to removal of or damage to all four parathyroid glands
Persistent or recurrent high calcium levels due to a parathyroid gland that could not be found during surgery or another parathyroid gland that becomes overactive after surgery.

