Skull base surgery is a specialized procedure used to remove benign and cancerous growths, cerebrospinal fluid leaks as well as abnormalities located on the underside of the brain, skull base, or upper vertebrae of the spinal column.
Given the complexity of this area, minimally invasive endoscopic techniques are often used. Surgeons can access the skull base by:
- Inserting instruments through natural openings(such as the nose or mouth)
- Making a small incision above the eyebrow
These advanced techniques allow for greater precision, reduced recovery time, and minimal scarring, making skull base surgery a highly effective approach for treating difficult-to-reach conditions.
Overview
The skull base is a specialized area of clinical work. The ENT surgeon is actively involved in this area, often as part of a team including a neuro surgeon or plastic/craniofacial surgeon.
Access to these difficult areas has increased with the development of image guidance systems and the ability to extend endoscopic sinus surgery approaches via the sphenoid to the skull base.
Acoustic Neuroma
An acoustic neuroma is a benign, slow growing tumour. It is more correctly called the vestibular schwannoma, because of its origin on the vestibular nerve. Post mortem data show that tumor is under diagnosed. An acoustic neuroma may be an incidental finding on MRI. Acoustic neuromas account for 6% of all intracranial neoplasms, the majority of which are sporadic (95%). 5% are genetic part of the inherited condition of NF2 on chromosome 22.
Acoustic Neuroma Presentation
The patient may experience some of the following:
- Sudden SNHL or progressive high frequency SNHL.
- Vertiginous episodes but these are rare as the patient unknowingly compensates.
- Symptoms of raised intracranial pressure such as headache or visual disturbance.
- Brainstem compression ataxia is a late symptom.
Acoustic Neuroma Investigations
- PTA
- MRI scan with gadolinium contrast.
- Full otoneurological exam.
- Hitselbergers sign postauricular numbness due to facial nerve compression.
- Reduced corneal reflex.
- Unterberger’s test positive patient marches on the spot with the eyes closed. A positive test is a rotation to one side or the other.
Acoustic Neuroma Management
Management options balance the risk of hearing loss, facial nerve palsy and surgical morbidity. There are several possibilities:
- Watchful waiting with serial MRI scans for slow growing tumours.
- Retrosigmoid approach: preserves the hearing
- Translabyrnthine approach: destroys the hearing but is an easier approach. It is useful if there is little hearing to preserve.
- Middle fossa approach: is technically challenging as it involves opening. the middle fossa. No driving for one year due to the risk of fitting.
- Intracapsular removal: useful to decompress large rumours in elderly patients with brainstem compression.
- Stereotactic radiosurgery this multiplanar radiotherapy is useful in small tumours as avoids surgery.
Acoustic Neuroma Complications
- Any intracranial procedure e.g. craniotomy-carries a 1% risk of mortality.
- Facial nerve palsy.
- Total hearing loss.
Nasopharyngeal Carcinoma (NPC)
There are two distinct types of this cancer of the back of the nose.
- Undifferentiated non-keratinizing squamous cell carcinoma (SCC) this is more common in people from southern China and Chinese people from Hong Kong. It is associated with EBV.
- Differentiated keratinizing squamous cell carcinoma (SCC) this has similar at risk groups to the majority of head and neck cancers.
Presentation
- Epistaxis
- Nasal obstruction
- Lymph node metastasis
- Middle ear effusion
- Extensive tumours can involve the skull base and cause cranial nerve palsies.
Investigations
Patients will be given a CT or an MRI scan.
Important
Every patient presenting with a unilateral middle ear effusion must have their postnasal space visualized to exclude an NPC.
Treatment
Radiotherapy is given for all stages. Neck dissection may be necessary there are extensive lymph node metastases.
Juvenile Angiofibroma
It is a rare tumour almost exclusively seen in males. (If the patient is female consider chromosomal analysis.) It originates from the sphenopalatine foramen and is locally invasive but not malignant. It is a combination of fibrous tissue with endothelial spaces in vascular tissue.
Juvenile Angiofibroma Presentation
- Recurrent epistaxis in young male (average age 14)
- Large posterior nasal mass
- Pulsatile mass palpated prior to adenoidectomy
- Nasal obstruction.
Juvenile Angiofibroma Investigations
- Clinical examination with endoscope
- CT scan and MRI scan
- Angiography
- A biopsy is avoided for fear of life threatening haemorrhage
Juvenile Angiofibroma Management
The treatment is surgical removal, with pre-operative embolisation to reduce the blood loss during the operation. There are several ways to gain access to the area, Initially most prevalent now is endoscopic approach.
Sinonasal Malignancy
It term describes a diverse group of malignant tumours affecting the nose and sinus system. SCC account for 70% of sinonasal malignancy. adenocarcinoma 10%, and adenoid cystic carcinoma 10%.
Nickel workers are at risk of developing SCC, woodworkers are at risk of adenocarcinoma. This is often delayed up to 20 years after exposure. The prognosis is poor with less than 50% of patients surviving for 5 years.
Common sites for sinonasal malignancy are:
- Maxillary sinus
- Nasal cavity
- Ethmoid sinus
Sinonasal Malignancy Presentation
Some or all of the following features may be seen:
- Nasal obstruction
- Epistaxis
- Sinusitis
- Maxillary symptoms
- Loose teeth
- Ulcer on palate
- Cheek swelling
- . Ethmoid symptoms
- Unilateral obstruction
- Diplopia
Sinonasal Malignancy Investigations
- CT scan or MRI scan
- Endoscopy and biopsy
- FNA if cervical metastases
Sinonasal Malignancy Treatment
Surgical resection or radiotherapy may be required. Treatment decisions should be made by an MDT in a specialist head and neck clinic taking into account the type of tumour and the staging.
Pituitary surgery
What is Pituitary Surgery?
Pituitary surgery is a procedure to remove tumors from the pituitary gland, a small gland located at the base of the brain that regulates hormones.
Why is it needed?
Surgery is often necessary for hormone-secreting tumors, non-hormone secreting tumors that cause headaches or visual disturbances, and cancerous tumors.
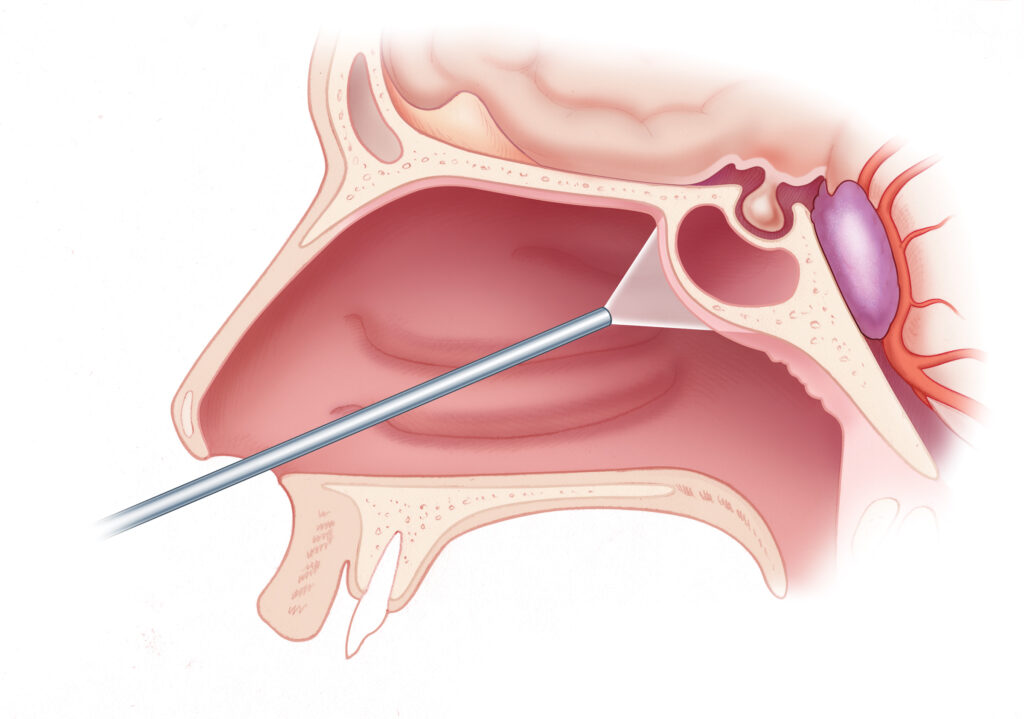
Transsphenoidal Approach
The most common approach is transsphenoidal surgery, where the surgeon accesses the pituitary gland through the sphenoid sinus (a hollow space behind the nasal passages) endoscopically.
What it is Invasive fungal sinusitis?
Invasive fungal sinusitis is a serious fungal infection of the nasal and sinus lining that can spread to surrounding tissues, including the eyes and brain, potentially leading to blindness or death, particularly in those with weakened immune systems.
Invasive fungal sinusitis Types?
Acute invasive fungal sinusitis: A rapidly progressing and potentially life-threatening infection that can spread quickly to the eyes and brain.
Chronic invasive fungal sinusitis: A slower-progressing infection that can sometimes mimic other types of sinus infections.
Chronic granulomatous invasive fungal sinusitis: A rare type of chronic invasive fungal sinusitis.
Invasive fungal sinusitis Causes
- Inhaling certain types of fungi.
- Weakened immune systems, which can allow fungi to invade tissues.
- Conditions like diabetes can increase the risk.
What is Cerebrospinal fluid (CSF)
- Cerebrospinal fluid (CSF) is a clear, colorless fluid that surrounds the brain and spinal cord, acting as a protective cushion.
- It helps regulate temperature and blood supply to the central nervous system and is part of the structural support for both the brain and spine.
What causes a Cerebrospinal Fluid (CSF) Leak?
- CSF leaks typically occur when there’s a tear or hole in the dura mater, the outermost layer surrounding the brain and spinal cord.
- This can be caused by various factors, including:
- Trauma: A blow to the head or spinal cord can create a tear in the dura.
- Iatrogenic: Post sinus surgery or skull base surgery, where CSF leak can happen from nose. Post mastoid or lateral skull base surgery where csf can leak from ear or it can prevent from nose to eustachian tube (tube connects the middle ear to the nasopharynx)
- Spontaneous Leaks: In some cases, there no clear cause or triggering event, and the leak may occur spontaneously, possibly due to a weakened or torn dura most commonly in middle aged, older adults, females, and those who are overweight or have connective tissue disorders.
- Underlying Conditions: Certain genetic disorders like Marfan Syndrome and Ehlers-Danlos syndrome can increase the risk of CSF leaks due to weakened connective tissues.
What is Cerebrospinal fluid (CSF) Rhinorrhea
Cerebrospinal fluid (CSF) rhinorrhea is a condition where the fluid that surrounds the brain leaks into the nose. It can be caused by head trauma, surgery, or birth defects.
Symptoms Runny nose and Watery discharge from the nose.
Risk
- CSF rhinorrhea can lead to dangerous infections like meningitis and brain abscess.
Treatment
- Conservative management includes bed rest with the head elevated, and avoiding coughing, sneezing, nose blowing, and heavy lifting.
- Endoscopic Surgery is used to repair the leak, decision for surgery is taken as per the condition of disease and patient.
Diagnosis
- A beta-2 transferrin test can help detect CSF in nasal mucus.
- Beta trace protein test can also help in diagnosis csf.
- A glucose test can help detect CSF in nasal mucus.
- A computed tomography (CT scan/MRI scan) scan to detect the breach in skull base and also to detect tumor / cancer.
Cerebrospinal fluid (CSF) otorrhea
Cerebrospinal fluid (CSF) otorrhea is a condition that occurs when spinal fluid drains from the ear. It can be life threatening and requires prompt medical care.
Symptoms
- Clear fluid draining from the ear
- Hearing loss in the affected ear
- Feeling like you’re in a tunnel, underwater, or in a barrel
Causes
- Skull fracture
- Tumor
- Infections
- Congenital anomalies
- Operative trauma
- A dural and bony defect in the tegmen area
Diagnosis and treatment
- A doctor may see fluid behind the eardrum
- A CT scan of the temporal bone may be ordered to identify the site of the leak
- Surgery may be required to repair the leak

